ACTIVE RESEARCH PROJECTS
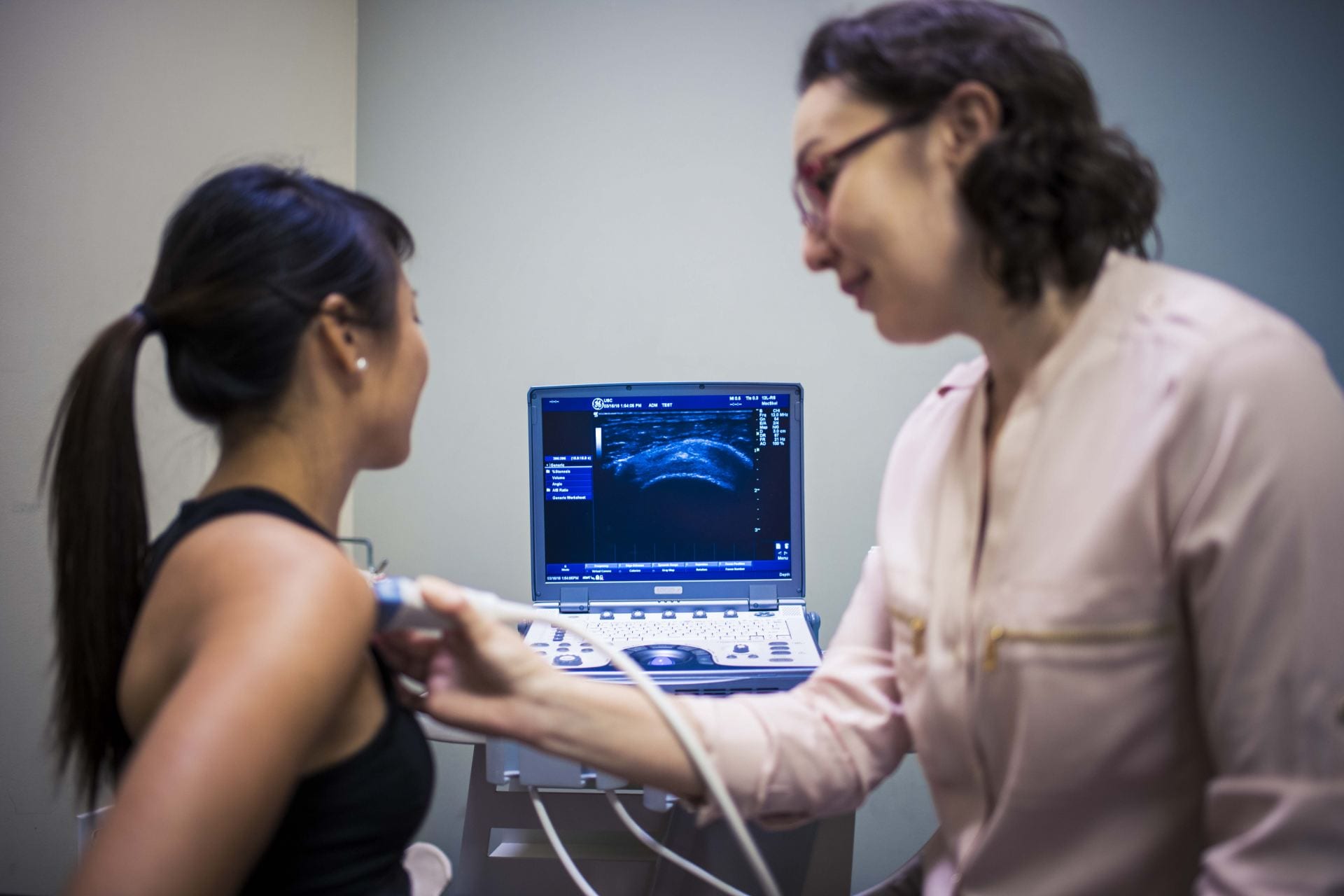
The purpose of this clinical trial is to identify mechanisms associated with a therapeutic response to resistance exercise in patients with rotator cuff tendinopathy. We look to characterize the peripheral factors of tendon structure and muscle performance, central factors of psychological status (e.g., pain catastrophizing, fear avoidance, pain self-efficacy) and brain activity in sensorimotor and pain processing areas. The findings will optimize the delivery and treatment response for exercise for patients with rotator cuff disease.
See more detail on our Exercise Study page.
Funding:
NIH/ NIAMS – R01AR083626 2024 – 2027
Patient-Specific Factors of Recovery in Rotator Cuff Tendinopathy
Resistance exercise is a known effective treatment for rotator cuff tendinopathy, but not for everyone. Defining the tendon structural response to exercise will define tendon recovery and its relationship to patient outcomes. Characterizing how mediating factors of muscle deficits, the brain’s pain and sensorimotor processing, and psychological factors influence the relationship between tendon recovery and patient outcomes will enable a patient-specific approach to rehabilitation.
Foundation for Physical Therapy Research 2023 – 2024
Biomarkers of Tendon Recovery for Rotator Cuff Tendinopathy
Define tendon morphological changes with 4-week resistance exercise, how the associated muscle modulates tendon remodeling, and the relationship to patient-rated outcomes in patients with rotator cuff tendinopathy.
Co- investigators:
Jason Kutch, PhD
The ulnar collateral ligament (UCL) provides ~50% of the counter to elbow varus torque during pitching, putting it at risk for injury. Varus torque increases with faster ball velocity during pitching, but not for all pitchers. We hypothesize that physical factors of movement quality and quantity of the shoulder, trunk and hip movement are able to moderate the forces transmitted to the elbow during pitching. The goal of this project is to define the ball velocity-elbow varus torque relationship, and the level by which physical factors can moderate this relationship to reduce elbow torque. A player profile for UCL injury risk developed for each pitcher can be used in 3 ways; to target the identified physical factors for prevention and rehabilitation after injury, specify return to sport criteria, and guide performance enhancement.
Read more about this study at HSC News.
Status: Active Enrollment
Co- Principal investigators:
Andrew Karduna, PhD
Co-investigators:
Roksana Karim, PhD
Collaborators:
Paul Diaz, ATC; Head Athletic Trainer for USC Baseball (USC)
Seth Gamradt, MD; Director of Orthopaedic Athletic Medicine, MD for USC Baseball (USC)
Tom Embree, ATC; Head Athletic Trainer for UO Baseball (UO)
Jeremy Vail, PT, ATC; Rehab Coordinator; Carl Stocklin, ATC, Head ATC, Baseball (UCLA)
Andrew Hawkins, PT, ATC; Minor League Rehab Coordinator. (Los Angeles Angels of Anaheim)
Funding Mechanism:
PAC-12 Student-Athlete Health and Well Being Grant. 2019 – 2022.
Multi-Site Institutions:
University of Southern California (USC), University of Oregon (UO), University of California, Los Angeles (UCLA)
The purpose of this study is to characterize the risk of upper extremity injury in baseball players based on preseason measures of shoulder range of motion, shoulder strength, and trunk/hip stability and strength. Besides, we aim to develop a streamlined screening battery of tests that can be used to identify risk factors associated with upper extremity injury.
Defining the deficits in the shoulder, trunk, and hip that prognosticate upper extremity injuries will lead to a better understanding of how these factors individually and in combination predict injury risk. The evidence-based screening exam can be used to identify injury risk, and those modifiable risk factors related to injury. Long-term, the goal is to leverage the findings of this study to develop pre-season and in-season prevention program to reduce injuries.
Status: Data Analysis/Manuscript Preparation
Co-investigators:
Hillary Plummer, PhD, ATC
Bernard Li, PT, DPT, OCS, SCS
Jonathan Sum, PT, DPT, OCS, SCS
Funding Mechanism:
Major League Baseball Research Grant. 2018 – 2019.
The purpose of this study are to determine the predictive validity of sonographic imaging as an early detection measure for work-related shoulder pain, and to determine the effects of first-time exposure to intensive work-related tasks on shoulder function, pain, strength, range of motion, nerve mobility, and tendon morphology.
Limited information exists regarding potential risk factors for the development of shoulder work-related pain and work-related musculoskeletal disorders. Early detection methods are needed to identify individuals at risk, in order to intervene before the development of shoulder pathology. By studying dental hygienist students we will be able to control for task-exposure, as all the participants will be exposed to similar profession-related tasks at the same time.
Status: Data Analysis/Manuscript Preparation
Co-investigators:
Shawn Roll, PhD, OT
Federico Pozzi, PhD, PT
Hillary Plummer, PhD, ATC
Catarina de Oliveira Sousa, PhD, PT
Funding Mechanism:
The Charles D. and Mary A. Bauer Foundation. $25,000. 2017 – 2019.
National Institute for Occupational Safety and Health / Centers for Disease Control (R01-OH010665). $2,324,186. 2015 – 2019.
For more info click here.
The purpose of this study is to determine the feasibility, acceptability, and patient-reported and performance outcomes of a 5-month closed-chain rehabilitation protocol for patients with full-thickness rotator cuff tears. Secondarily, the effects of the closed-chain rehabilitation protocol on, shoulder impairments, tendon morphology, and shoulder biomechanics will be assessed. These rehabilitation exercises, if demonstrated to be effective, could be used to direct treatment for future patients with rotator cuff tears.
Enrollment: Active
Status: Patient Enrollment
Do you have a rotator cuff tear?
We are inviting individuals between the ages of 40 and 85 who have a full-thickness rotator cuff or a failed rotator cuff repair and have not participated in physical therapy within the last 3 months.
For more information, please contact the COOR Lab:
COORlab@pt.usc.edu or call 323-224-5032
Funding Mechanism:
Barbara Fried, Fried Companies, Inc. 2015 – 2019
Shoulder dysfunction is prevalent in individuals with spinal accessory nerve injury. Spinal accessory nerve injury affects the muscle activity and function of the lower trapezius muscle.Weakness or paralysis of the trapezius muscle may cause a loss in shoulder and scapula motor control. However biomechanical factors such as tendon characteristics, shoulder mechanics and muscle activation during arm elevation are not well understood. The purpose of this study is to investigate shoulder function and muscle activity in patients with spinal accessory nerve injury.
Enrollment: Active
Status: Patient Enrollment
Co-Investigators
Kimi Yamada, PT, DPT, OCS, ATC, CLT, CSCS
HEALTH SERVICES RESEARCH
Clinical Practice Guidelines (CPGs), such as those developed by the Orthopaedic Section, were written to enable clinical decision-making. Shoulder pain is a common complaint, and rotator cuff (RC) disease is the most prevalent shoulder diagnosis.Recently, evidence-based CPGs have been published for RC disease, but to guide clinicians in the treatment of RC disease. While these CPGs are evidence-based, there is a lack of evidence as to the effects of adherence to the CPGs on patient-rated outcomes, and the relationship to dose of care. This project will convert clinical data into meaningful data elements to define CPG adherence for RC disease, and define the relationships to patient outcomes and dose of care.
Enrollment: NA
Status: database acquisition
Funding: Orthopaedic Section of APTA; Clinical Research Network (CRN) Grant, 2017 – 2019
Co-Investigators
Co-PI: Chuck Thigpen, PhD, PT, ATC
Co-Investigators
Chad Cook, PhD, PT, FAAOMPT
Federico Pozzi, PhD, PT
Funding Mechanism:
Orthopaedic Section of the APTA. 2017- 2019.