Clinical history
- 51 years old female presented for follow up on liver lesions seen on CT scan .
- Patient has a complicated past medical history including, Cushing’s Disease, due to ACTH-secreting pituitary adenoma, status post transsphenoidal resection (1990), with refractory hypercortisolism, and chronic adrenal insufficiency, status post bilateral adrenalectomy, showing incidental metastatic renal cell carcinoma/ clear cell type (2011), status post left nephrectomy (2013).
- Patient also has a history of papillary thyroid carcinoma with pulmonary metastasis, status post total thyroidectomy (2014), with multiple following neck dissections showing metastatic PTC on (2014 & 2015) with radioiodine treatment (2016), leading to postsurgical hypothyroidism,
- Other medial problems include type II diabetes, hypertension, osteopenia, and seizure.
Initial workup
- The previous CT scan showed a 2 cm hypoenhancing lesion at the liver dome.
- Following Multiphase liver CT scan with contrast showed Interval increase in size of the lesion to 22.45 mm hypodense mass in the medial hepatic dome, highly suspicious for metastatic disease in this patient with history of papillary thyroid cancer (figuer1).
- There was also a new 14 mm hypodense in the lateral left hepatic lobe which was also suspicious for metastatic disease. The patient was referred for fine needle aspiration.

Fine Needle aspiration findings
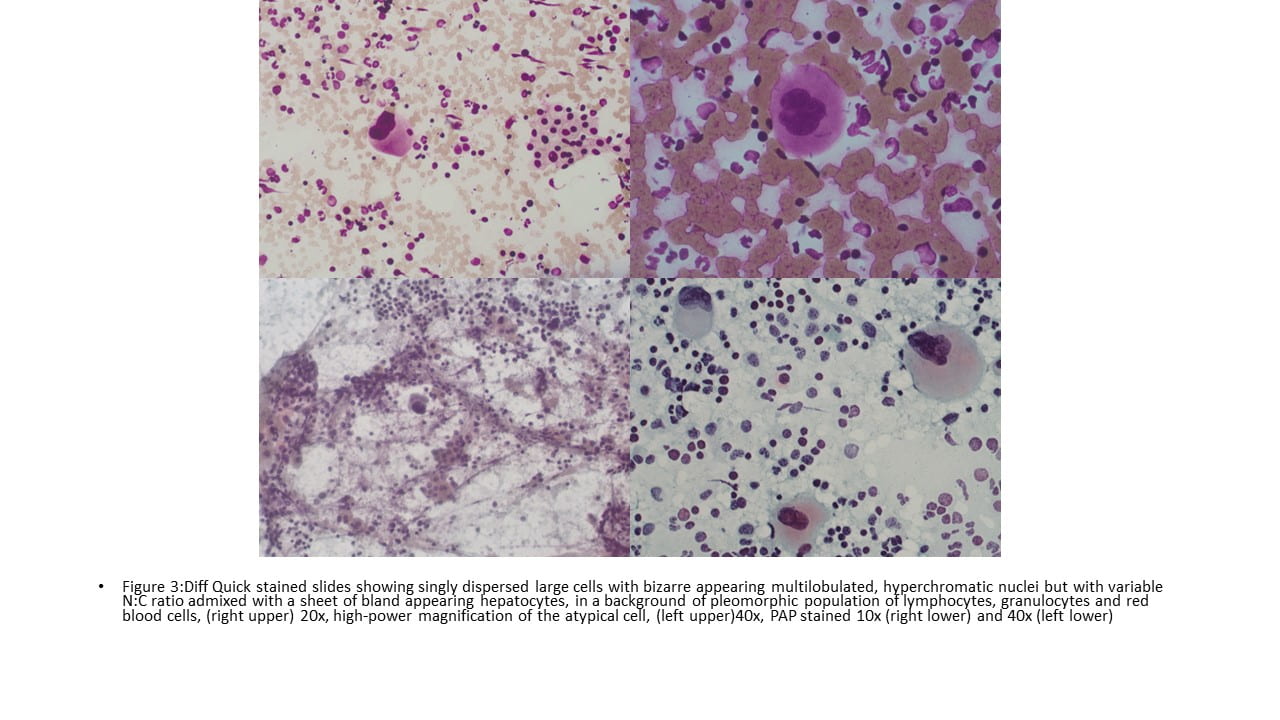
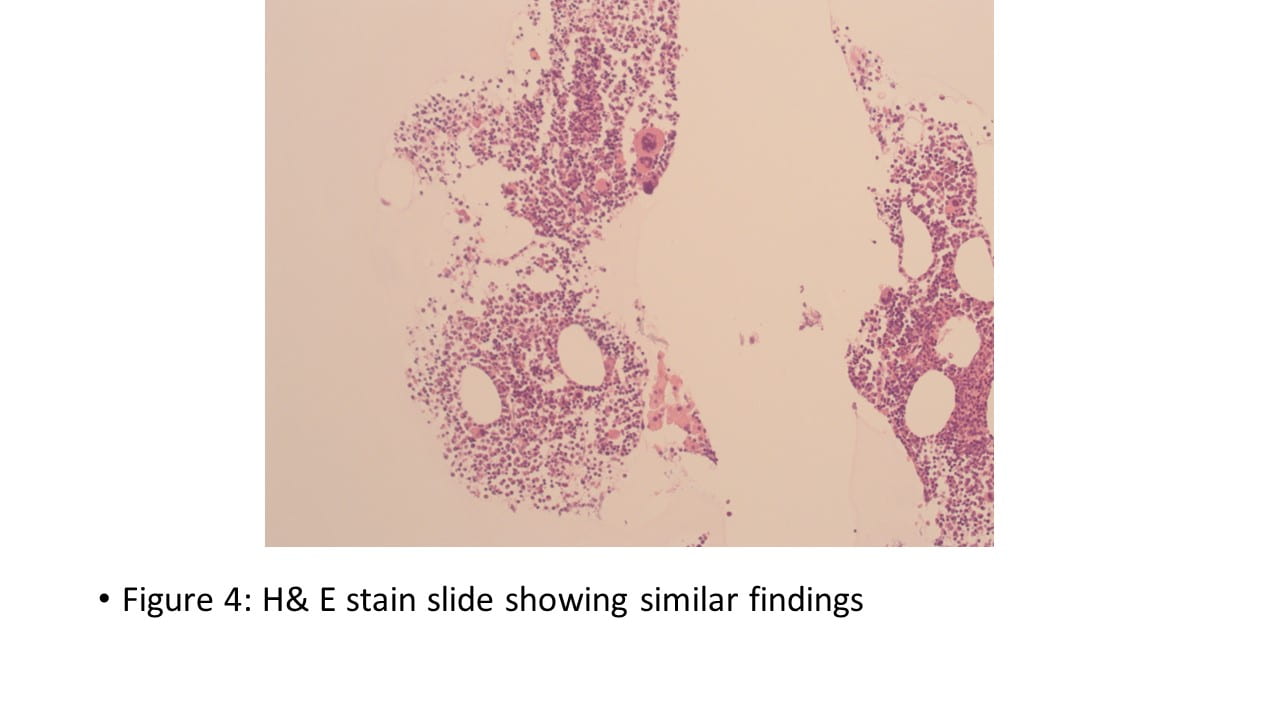
- Smear preparations were cellular showing numerous singly dispersed large cells with bizarre appearing multilobulated, hyperchromatic nuclei but with variable N:C ratio, admixed with pleomorphic population of lymphocytes and granulocytes. The background consists of aggregates and small sheets of hepatocytes, macrophages, and red blood cells. The cell block is less cellular but otherwise shows similar findings (figure 2-4).
 IHC Stains
IHC Stains
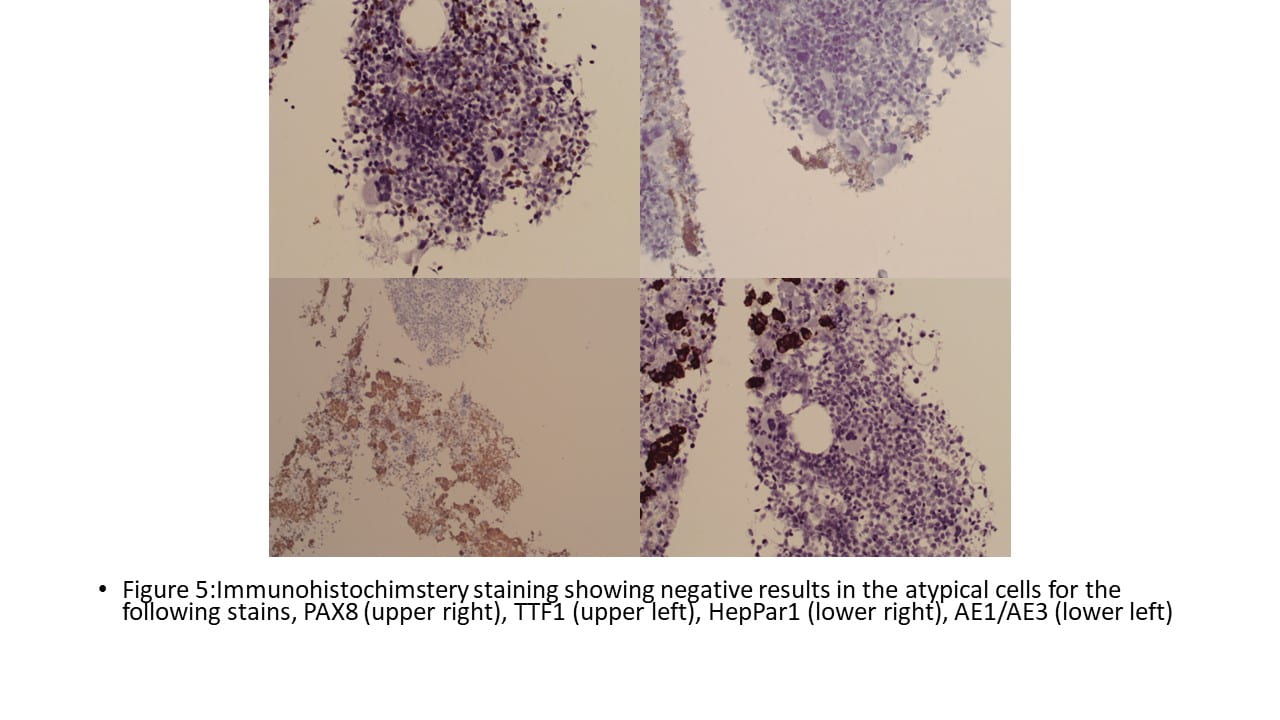
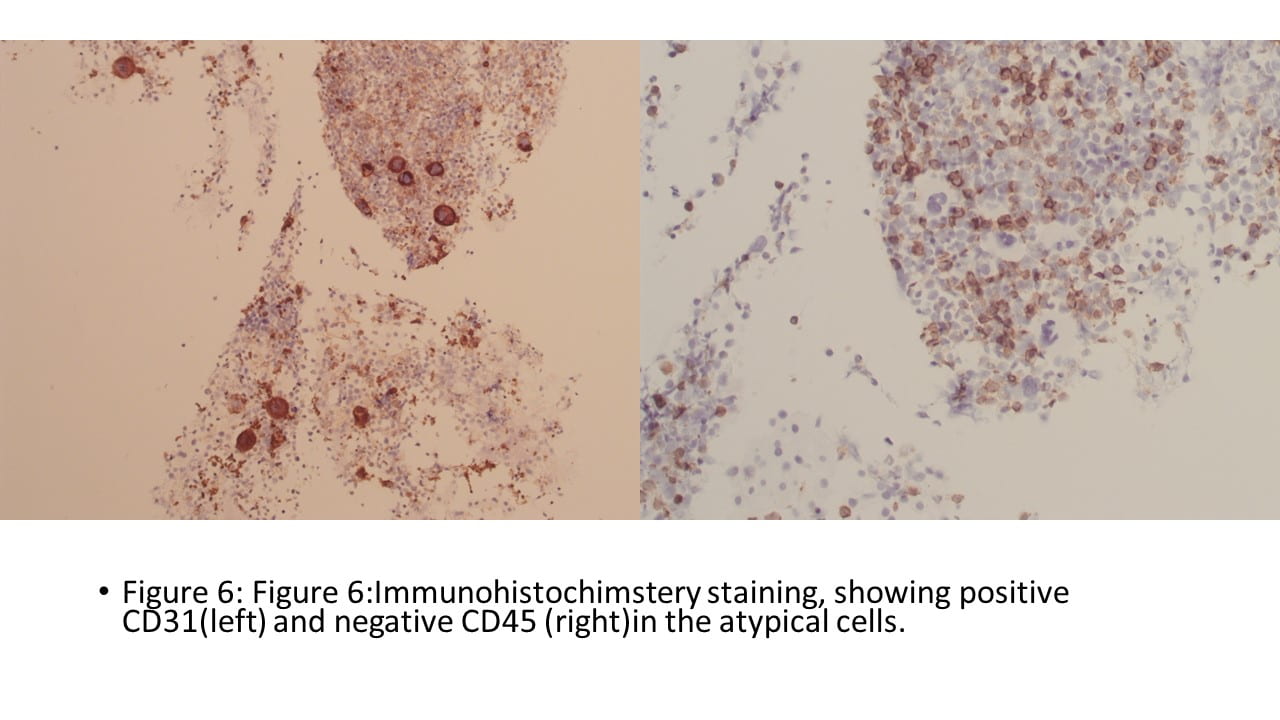
- Immunohistochemical stains were performed on the cell block and show the following results: Pancytokeratin, TTF-1 and HepPar1 were negative in the atypical cells but positive in hepatocytes. PAX8 and CD45 are negative in the atypical cells and positive in small lymphocytes. CD31 is positive in the atypical cells (figure 5 & 6).
 Final Cytologic diagnosis
Final Cytologic diagnosis
- The overall cytomorphology and Immunohistochemical pattern of staining were consistent with the presence of polymorphic lymphoid/granulocytic population and megakaryocytes.
- This may be seen in extramedullary hematopoiesis or in myelolipoma, both of which may be included in the differential diagnosis. Definitive cytologic features of malignancy are not identified.
Discussion
- Hematopoiesis usually occurs in bone marrow in adults and when it occurs at sites except for bone marrow, it is known as extramedullary hematopoiesis (c). It is typically seen in organs that are vigorously involved in fetal hematopoiesis, including liver, spleen, and lymph nodes. Seldom, it has also been recognized in other sites for instance mediastinum, paraspinal/paravertebral region, adrenal, lung, pleura, gastrointestinal tract, kidney, prostate gland, breast, and so forth1.
- EMH is a compensatory mechanism that is closely related to inadequate functioning of medullary hematopoiesis, especially myeloproliferative disorders and hemolytic anemia. However, there have also been reports of EMH in cases of malignant solid tumors, including breast cancer, lung cancer, and Kaposi’s sarcoma2
- EHM is rarely presents in the liver, especially as liver mass and only very few liver nodules of EMH have been described in the literature.
- The etiology of EMH in patients with solid tumors remains unclear. Granulocyte colony-stimulating factor (G-CSF) may be an inducing factor of EMH2.
- Screening the smear at low power is crucial in such cases, as megakaryocytes are more readily seen at low power. These cells are so peculiar that they “stare at” the cytopathologists. Though megakaryocytes have distinct morphology still they can be confused with atypical cells. Therefore, awareness of their morphology is critical for the basic diagnosis1.
- Our case presented with a complicated past medical history including pituitary adenoma, metastatic renal cell carcinoma/ clear cell type and papillary thyroid carcinoma with pulmonary metastasis.
- The patients 2.2 mm liver nodule was thought to be a result of metastasis for one of the mentioned tumor. During rapid on-site evaluation, the presence of the large atypical cells on the Diff Quick stained concluded the specimen as adequate.
- Our smear and H & E slides showed numerous singly dispersed large cells with bizarre appearing multilobulated, hyperchromatic nuclei but with variable N:C ratio. These cells were the clue for the diagnosis as they showed significant similarity to Megakaryocytes seen usually in the bone marrow.
- Above finding also seemed sensible to the cells presented in the background, which included pleomorphic population of lymphocytes, and granulocytes, macrophages, and red blood cells
- Multiple sheets and singly dispersed population of bland appearing hepatocytes were also present in the background, and they look very district form the atypical cells.
- Immunohistochemical stains were performed to exclude any poorly differentiated carcinoma (Pancytokeratin), including papillary thyroid carcinoma (TTF-1), renal cell carcinoma/ clear cell type (PAX8) and primary hepatocellular carcinoma (HepPar1), and all were negative in the atypical cells. Also, (CD45 ) was performed to exclude any lymphoma (CD45) and results are also negative in the atypical cells, but positive in the background small lymphocytes.
- CD31 was the only positive stains (granular, membranous expression) in the atypical cells which confirmed our cytomorphological impression.
- It is usually unnecessary to treat asymptomatic patients with EMH, whereas there are several options for the treatment of symptomatic patients, including hydroxyurea, transfusion, radiotherapy, and surgery.(2)
- Our patient did get any further treatment for the liver lesion, as the lesion did not case any symptom.
References
1.Kapatia G, Kaur A, Rastogi P, et al. Extramedullary hematopoiesis: Clinical and cytological features. Diagnostic Cytopathology. 2020;48:191–196. https:// doi.org/10.1002/dc.24353
2.Bao Y, Liu Z, Guo M, Li B, Sun X, Wang L. Extramedullary hematopoiesis secondary to malignant solid tumors: a case report and literature review. Cancer Manag Res. 2018;10:1461-1470
https://doi.org/10.2147/CMAR.S161746