- 56-year-old male with past medical history of Diabetes Mellitus, T2a cutaneous T cell lymphoma/mycosis fungoides, and stage III clear cell renal cell carcinoma status-post left nephrectomy in December 2018. Pathology report of the nephrectomy specimen revealed an 8 cm mass with clear cell renal cell carcinoma, histologic grade 4 with about 10% sarcomatoid features. Thyroid ultrasound showed mixed cystic and solid, isoechoic nodule measuring up to 1.5 cm (TIRADS 4).
- Ultrasound-guided fine needle aspiration of right thyroid nodule was performed.
- Diff-Quik preparation and pap stained smears showed pauci-cellular specimen with rare bland thyroid follicular cells arranged singly and in small groups with Hurthle cell changes, in a background of scant colloid, few macrophages, blood cells and debris. No malignant cells identified in the smears.
- Cell Block: showed two group of cells with irregular nuclei, prominent nucleoli, eosinophilic cytoplasm and cytoplasmic clearing.
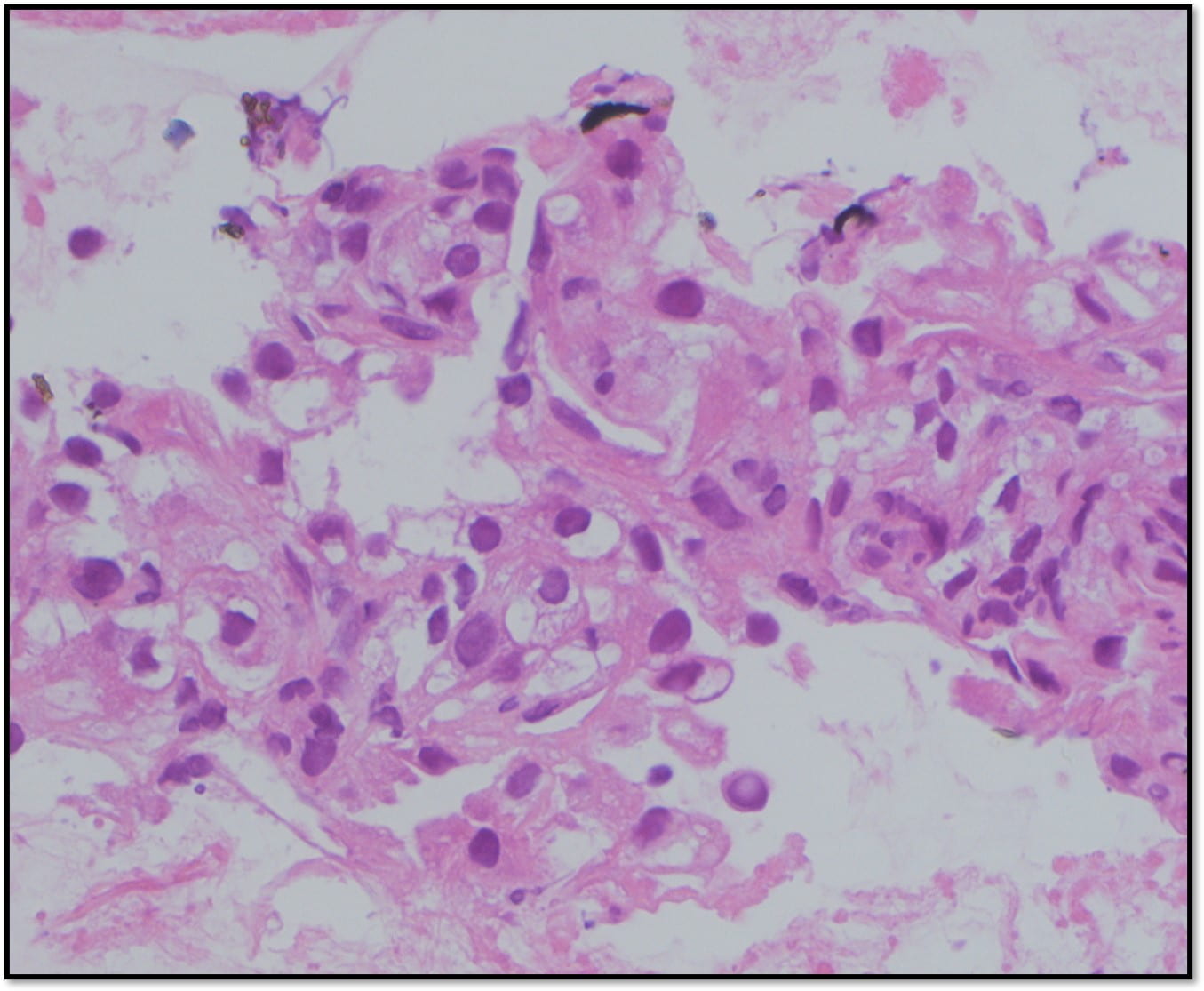
- Cell Block: showed two group of cells with irregular nuclei, prominent nucleoli, eosinophilic cytoplasm and cytoplasmic clearing.
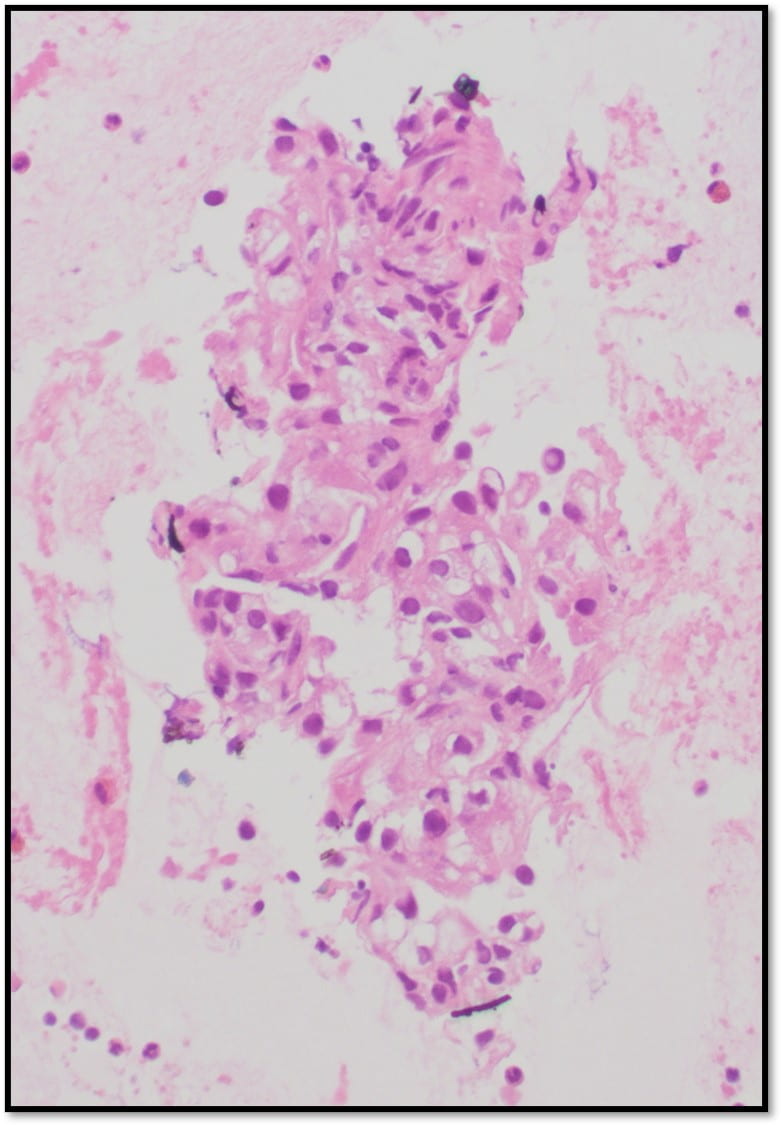
- Cell Block: showed two group of cells with irregular nuclei, prominent nucleoli, eosinophilic cytoplasm and cytoplasmic clearing.
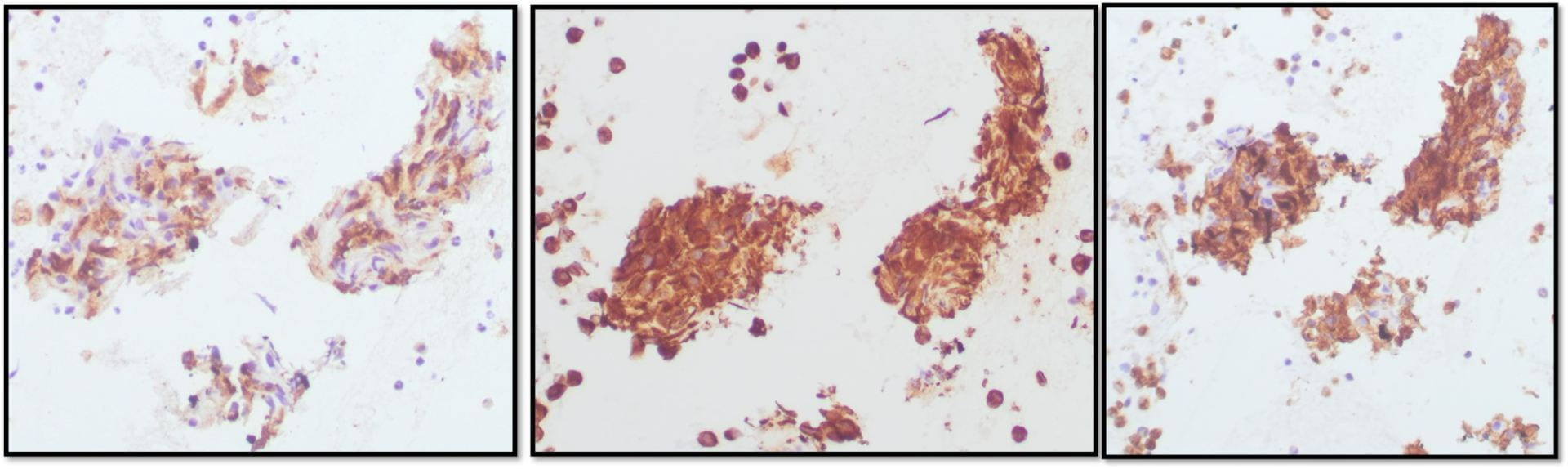 Positive RCC, CD10 and vimentin staining: compatible with RCC origin
Positive RCC, CD10 and vimentin staining: compatible with RCC origin
-
 Negative staining for TTF1 (specific stain for primary thyroid carcinomas and negative in metastatic RCC)
Negative staining for TTF1 (specific stain for primary thyroid carcinomas and negative in metastatic RCC)
Discussion
Clear cell renal cell carcinoma comprises 75%-80% of all RCCs and is strongly associated with a variety of deletions on chromosome 3p, the site for VHL gene. Size is not a determinant of malignancy, but the frequency of metastases does correlate with increasing size of the primary tumor. Cytomorphologic features of clear cell renal cell carcinoma include: large cohesive cell groups, abundant wispy cytoplasm with ill-defined edges, cytoplasmic vacuoles, large, round, eccentrically placed nucleus, nucleoli (vary in size depending on WHO/ISUP grade), and blood.
Despite its robust vascularity, metastases to the thyroid gland only account for a small proportion of benign and malignant thyroid entities diagnosed. The possibility of metastasis should be considered whenever the cytologic picture does not conform with common thyroid neoplasms or the patient has a history of cancer elsewhere in the body.
Definitive diagnosis of metastatic RCC to the thyroid can only be confirmed by immunohistochemical staining and histologic examination. FNA with ultrasound guidance is the most common approach. FNA sensitivity and specificity for diagnosing metastases to the thyroid have been reported to be as high as 94% and 100%.
When a metastasis is suspected, comparing the aspirated specimen to previous histologic or cytologic material is very helpful, as is immunohistochemistry. Immunohistochemical staining for markers specific to RCC are utilized including CD10, vimentin, cytokeratin 7, and renal cell carcinoma marker. It is also helpful to use staining markers for thyroglobulin, calcitonin, and thyroid transcription factor 1 (TTF-1), which are specific to primary thyroid carcinomas and negative with metastatic RCC.
References
- Cibas ES, Ducatman BS. Cytology: Diagnostic Principles and Clinical Correlates. Fifth Edition.
- Thomas Rand Geisbush, Zaneta Dymon, Medhat Sam Gabriel, and Vivek Yedavalli. A Multimodal and Pathological Analysis of a Renal Cell Carcinoma Metastasis to the Thyroid Gland 11 Years Post Nephrectomy. J Radiol Case Rep. 2019 Apr; 13(4): 1–9.Published online 2019 Apr 30. doi: 10.3941/jrcr.v13i4.3497
-
