Clinical History:
29-year-old female presented to the ED for 2-3 months of worsening lower abdominal pain. She had a lifelong history of monthly menses, previously lasting 6-7 days with moderate flow, but noticed that her periods became lighter and shorter the past 2-3 months as well. She reported a 12-pound weight loss over the last month but associated this with increased exercise. She also endorsed worsening dyspareunia, and denied abnormal vaginal discharge, constipation, blood in the stools, hematuria, nausea and vomiting.
Initial Work-Up:
CT revealed innumerable heterogeneously enhancing and centrally necrotic soft tissue masses and nodules scattered throughout the abdominal cavity and pelvis, involving the peritoneum, omentum, and left ovary, with the largest mass (10.2 x 9.3 x 8.0 cm) in the right lower quadrant adjacent to the right adnexa and possibly arising from the right ovary.
CA125 was elevated to 258 and CEA, CA19-9, AFP, estradiol, and testosterone were within normal limits. An endometrial biopsy (EMB) and pap were performed. The EMB showed benign proliferative endometrium and PAP was negative for intraepithelial lesion.
The patient then underwent ultrasound-guided biopsy of the right adnexal mass with adequacy evaluation performed by cytopathology at time of the procedure.
Cytology (touch preparations of the right adnexal mass core biopsy):
The Diff-Quik stained preparations showed a relatively monotonous population of moderately atypical cells with eccentric nuclei with increased nuclear to cytoplasmic ratios, occasional prominent nucleoli, smooth nuclear contours, and finely vacuolated cytoplasm, occurring singly and in few loosely cohesive groups (Fig. 1-3). Occasional binucleated forms were identified. In the background were numerous mixed inflammatory cells.
The touch preparation was called adequate with lesional cells present at time of procedure.
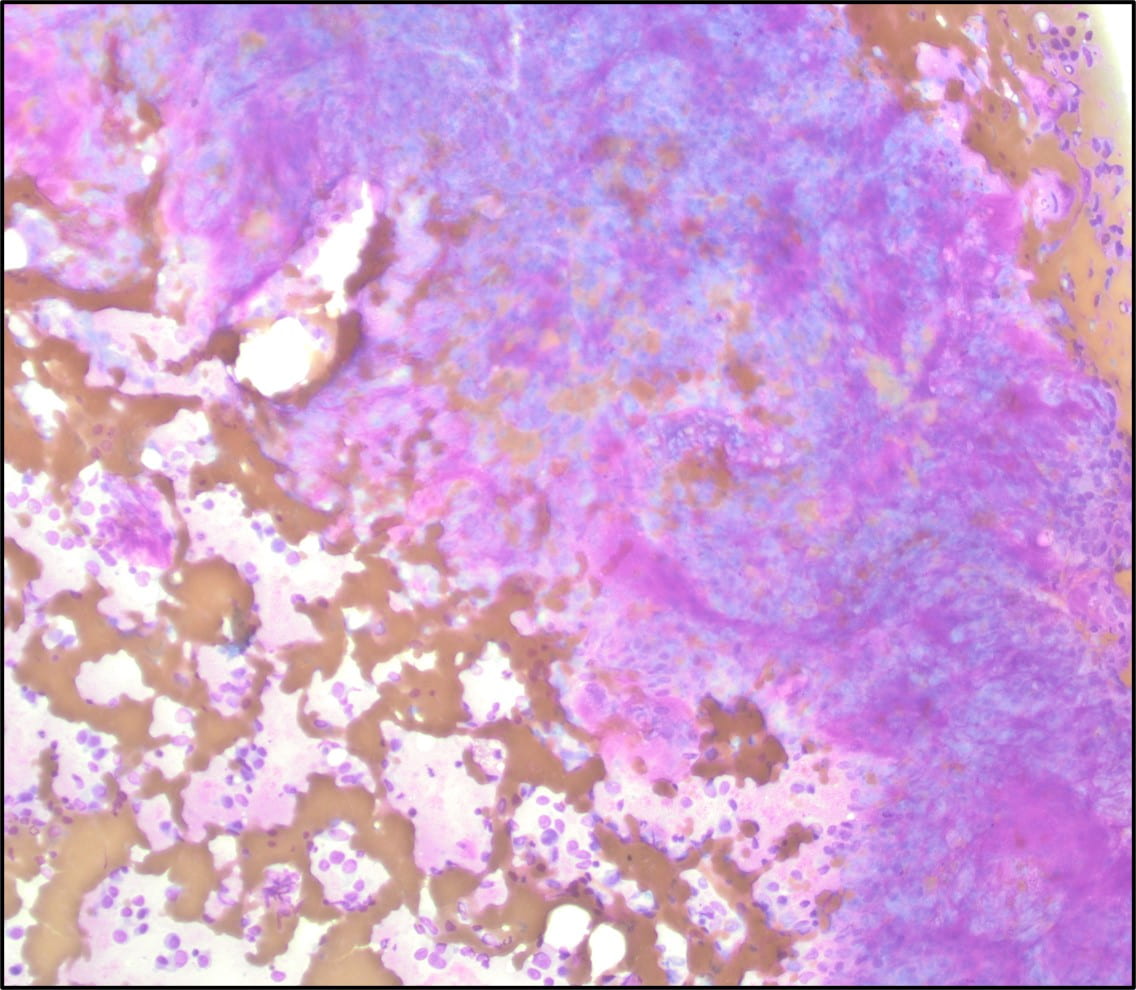
Figure 1: Diff Quik stained touch preparation showing numerous plasmacytoid cells (100x).
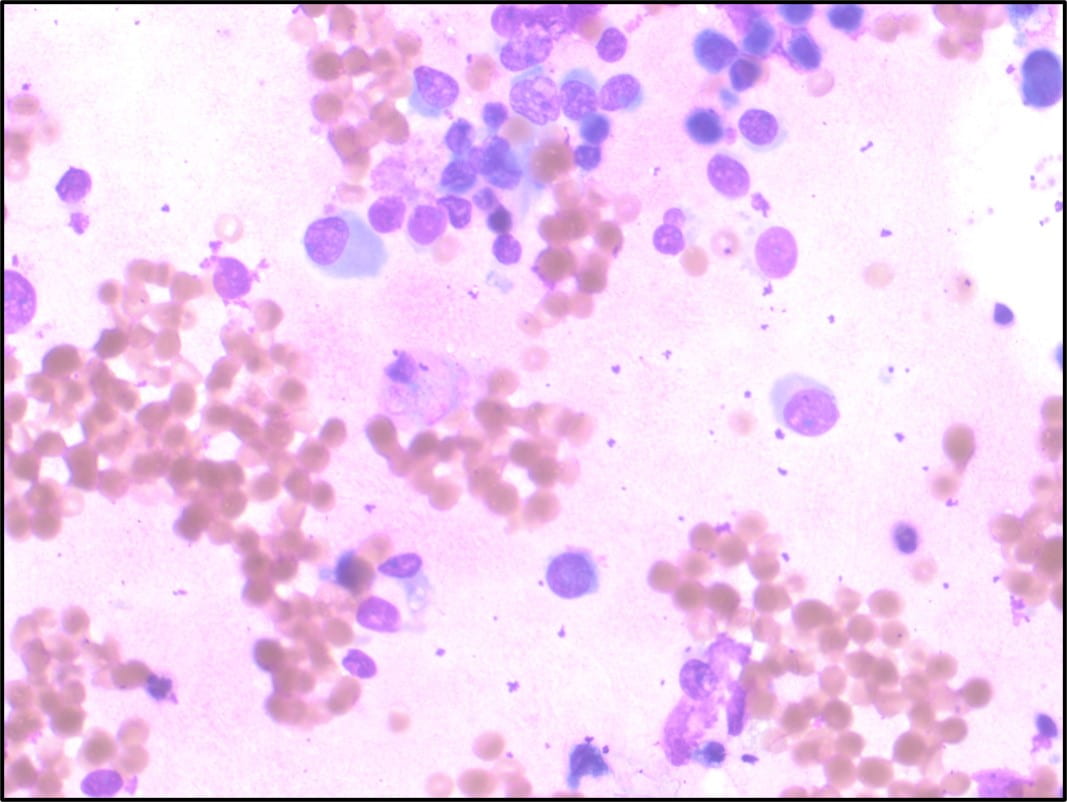
Figure 2: Diff-Quik stained touch preparation showing cells with eccentric nuclei, increased N:C ratio, and occasional prominent nucleoli occurring singly (400x).
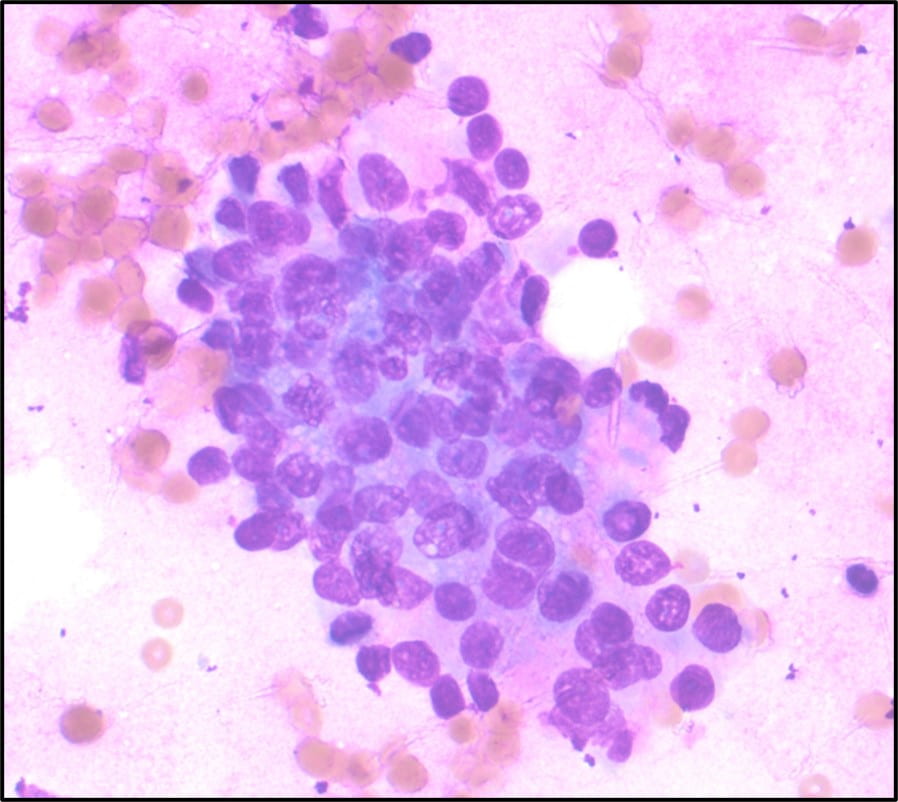
Figure 3: Diff-Quik stained touch preparation showing loosely cohesive group of cells with mild anisonucleosis and smooth nuclear contours (400x).
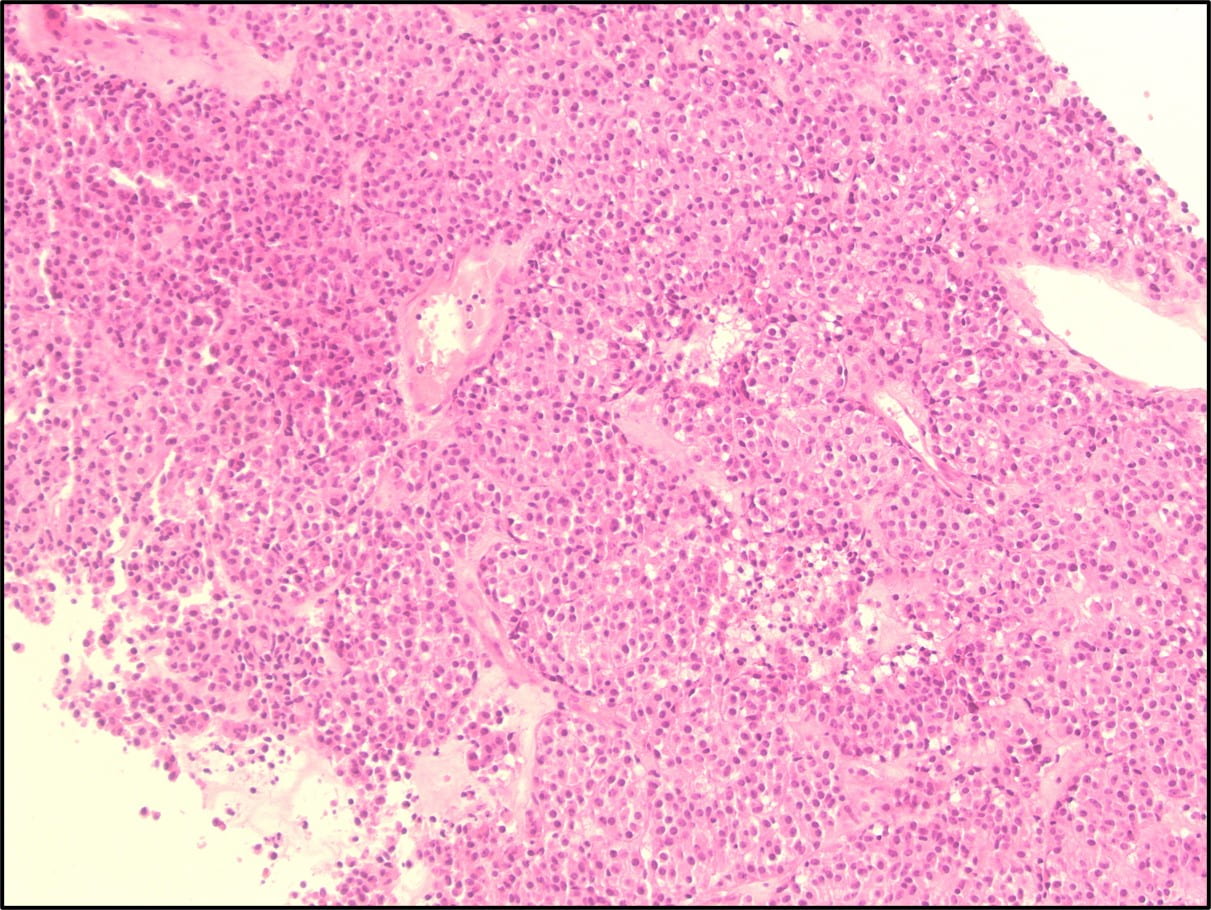
Figure 4: Core biopsy showing tumor cells arranged in nests and trabeculae (100x).
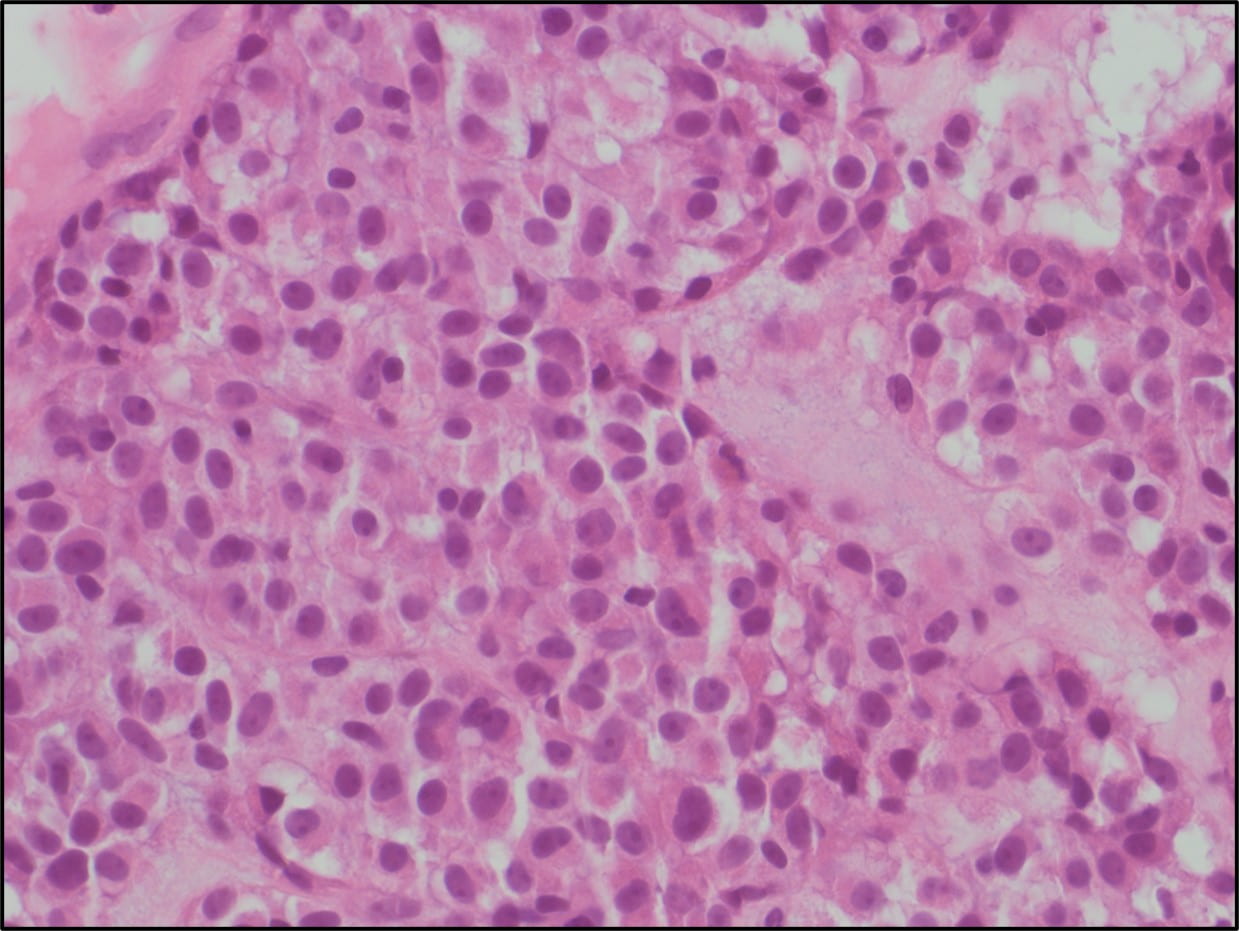
Figure 5: Core biopsy (400x)
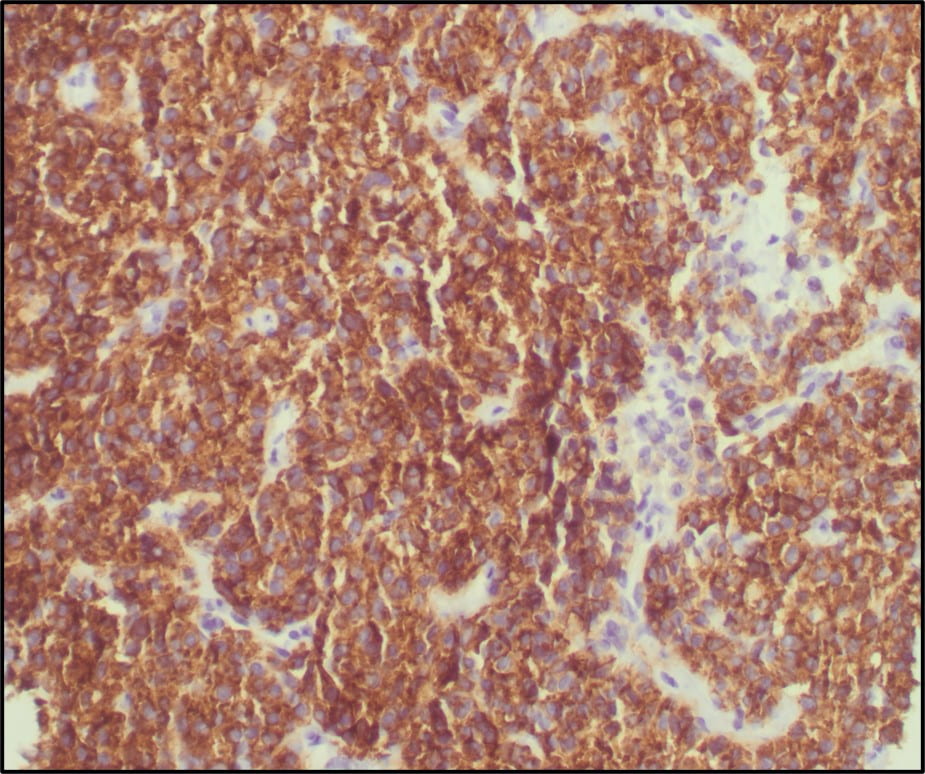
Figure 6: CD117 (200x)
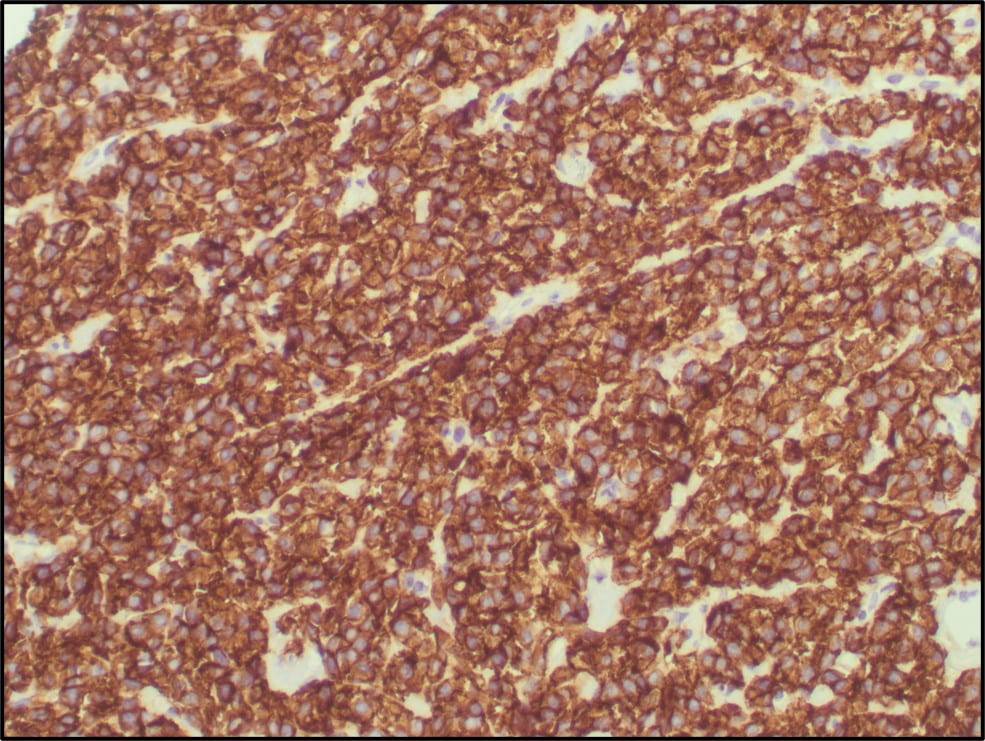
Figure 7: DOG1 (200x)
Core biopsy of right adnexal mass:
The core biopsy showed monotonous plasmacytoid cells with minimal pleomorphism, increased N:C ratios, and dense to flocculant cytoplasm, organized in nests and trabeculae (Fig. 4,5). Several mitotic figures were identified.
Diagnostic considerations included PEComa, ovarian sex cord or germ cell tumor, renal tumor, and lymphoma; however, PanCK, HMB45, S-100, PAX-8, CD45, Inhibin, SALL-4, and OCT-4 were negative. The tumor was also negative for desmin, synaptophysin, chromogranin, calretinin and p63. SMA was focally weakly positive, and Vimentin was positive. At this point, a gastrointestinal stromal tumor entered the differential, and the tumor showed positive expression for CD34, CD117 (Fig. 6), and DOG1 (Fig.7).
The case was signed out as predominantly epithelioid gastrointestinal stromal tumor.
Given the clinically malignant behavior of the tumor, the final touch preparation diagnosis was malignant cells present (correlate with the surgical pathology report for definitive characterization).
Patient Follow-Up:
The primary site remained indeterminant. The patient was re-admitted a couple months after initial presentation with imaging showing progression of disease. SDH mutational testing was requested and is pending.
Discussion:
Gastrointestinal stromal tumors (GISTs) are uncommon tumors of the GI tract that originate from the interstitial cells of Cajal, with a median age at presentation of 65 years. They typically arise in the stomach (56%), small bowel (32%), and colon and rectum (6%). Rarely, extra-gastrointestinal GIST can arise in the omentum, mesentery, retroperitoneum or pleura. Majority have activating mutations of c-kit. Those arising in younger individuals may contain mutations in one of the subunits of SDH, which can be seen in the setting of Carney Triad and Carney-Stratakis syndrome.
GISTs have three main histologic subtypes: spindled (most common), epithelioid, or mixed. The cytology generally shows spindled to epithelioid cells with bland chromatin and wispy cytoplasm arranged as large, crowded clusters of cells or occurring singly. Some cells may show perinuclear vacuoles (especially in gastric GISTs) . Definitive diagnosis is aided by IHC stains: about 95% show expression of CD117 and 88% show expression of DOG-1. SMA is generally negative but can be positive. S100 is negative. In SDH deficient GISTs, there is loss of SDHB expression.
Up to 40% of small intestinal GISTs and 25% of gastric GISTs behave malignantly. Prognosis depends on tumor size, site of origin, mitotic rate and presence or absence of intraoperative tumor rupture. Treatment generally entails surgical resection with tyrosine kinase inhibitors indicated in metastatic/recurrent GISTs.
References:
- Bell P, Findeis-Hosey J. GIST. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachGIST.html. Accessed March 4th, 2021.
- Cibas ES, Ducatman BS. Cytology: Diagnostic Principles and Clinical Correlates. Fifth Edition.
- Trisha M. Parab, et. Al. Gastrointestinal stromal tumors: a comprehensive review. Journal of Gastrointestinal Oncology. 2019; 10(1):144-154. doi: 10.21037/jgo.2018.08.20
