- 57 year old male with a past medical history of hypertension, type 2 diabetes, GERD, and asthma presented with 2 months of hemoptysis, weight loss, night sweats.
- Reports a history of positive PPD, but has never been treated for tuberculosis. Sputum cultures were AFB-negative x3.
- Imaging showed a partially calcified left hilar mass with extension and occlusion of the left lower lobe
- Patient underwent endobronchial ultrasound for further characterization of the mass and FNA sampling
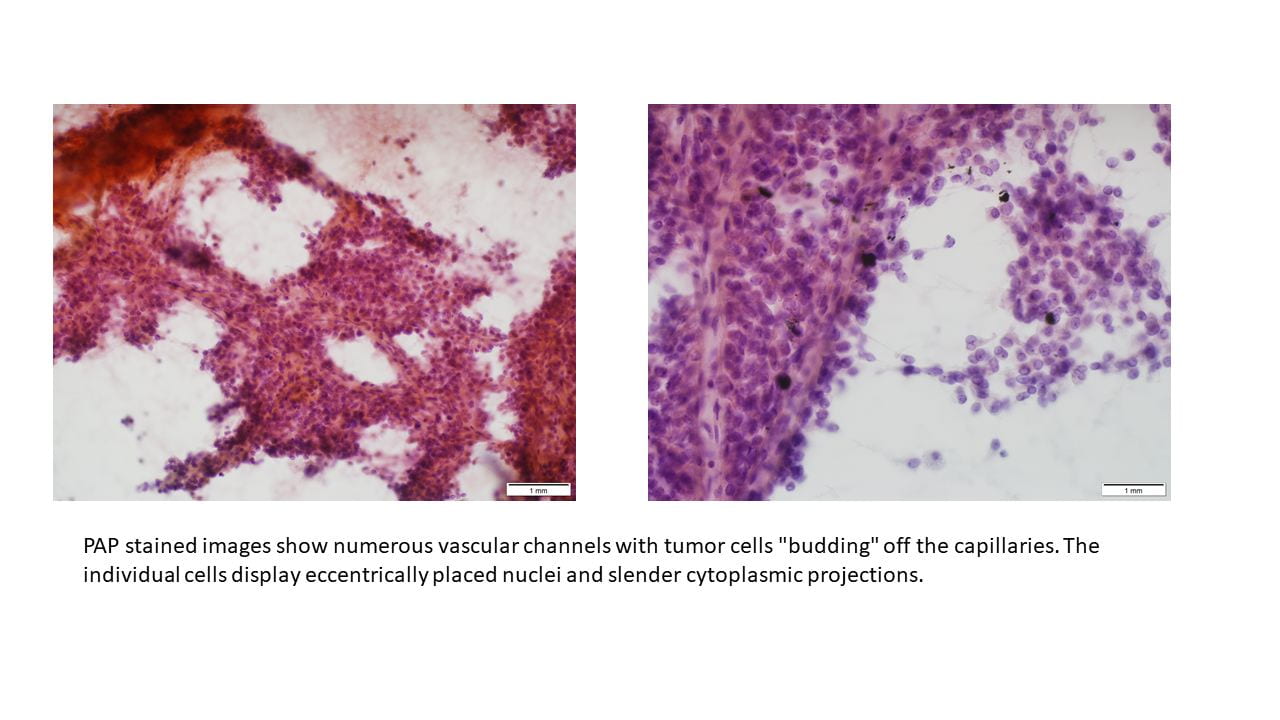
Microscopic findings, architecture & cytologic features:
Cellular smear preparations show numerous singly dispersed and loosely cohesive flat sheets of small atypical cells with high nuclear to cytoplasmic ratios, round to oval hyperchromatic nuclei, salt and pepper chromatin, rare mitotic activity (<2 per high power field), and scant granular cytoplasm in a background of numerous mixed inflammatory cells, ciliated bronchial epithelial cells, and acellular debris. Cell block findings consistent with smear preparations with rosette and nest formations seen.

Final Diagnosis: Carcinoid Tumor
Discussion
Pulmonary neuroendocrine tumors are divided into four classifications: carcinoid, atypical carcinoid, large cell neuroendocrine carcinoma, and small cell carcinoma. Of these entities, typical carcinoid tumors have the best prognosis. Carcinoid tumors are low-grade malignant neoplasms representing 2-3% of pulmonary tumors. Regional lymph nodes may be involved in 10 to 15% of patients and 5 to 10% will eventually have distant metastasis. Patients with typical carcinoid tumors may present with hemoptysis, cough, wheezing, and recurrent pneumonias. Carcinoid syndrome, characterized by flushing, diarrhea, wheezing, and hypotension, rarely occurs. Symptoms depend on the location of the tumor, as peripheral lesions are more likely to be asymptomatic, while central lesions may cause compression of nearby structures and post-obstructive pneumonias. On imaging, peripheral tumors present as a solitary pulmonary nodule, while central lesions may show evidence of compression to the airway and atelectasis. These lesions may also be calcified.
Typical features of carcinoid tumors on cytologic preparations include uniform appearing cells, isolated and in loose clusters. The tumor cells may range from round to oval or elongated and generally have moderate to abundant granular cytoplasm. The nuclei are round with smooth contours and contain “salt and pepper” chromatin. On histologic and cell block sections, the tumor cells may form nest, ribbons, papillae, or rosettes. The typical cytologic features and formations seen on the cell block sections are are consistent with those seen in the case.
The differential diagnosis of carcinoid tumors includes benign bronchial epithelial cells, adenocarcinoma, lymphoma, and other neuroendocrine tumors including atypical carcinoid tumor and small cell carcinoma. Carcinoid tumor cells may appear similar to benign bronchial cells as they have a bland appearance that mimics normal cells, but they will not be ciliated. They may be mistaken for adenocarcinoma due to their propensity to form rosette structures. Carcinoid tumor cells may be distinguished from lymphoid cells by their more abundant cytoplasm. The different pulmonary neuroendocrine tumors must be distinguished from each other by the number of mitotic figures per high-powered field. Typical carcinoid tumors have <2/hpf, atypical carcinoid tumors have 2-10/hpf, and large cell neuroendocrine carcinomas and small cell carcinomas will each have >10/hpf. Immunohistochemical stains are also important in narrowing the differential diagnosis. Chromogranin and synaptophysin stains can readily distinguish tumor cells of neuroendocrine origin and are important in making the diagnosis of carcinoid tumor. Most carcinoid tumors are also positive for keratins, as in this case. TTF-1 may be positive in about a third of carcinoid tumors but was negative in the case. The most important stain in distinguishing carcinoid tumor from other neuroendocrine tumors is Ki-67, a marker for mitotic activity. Less than 25% of cells will stain positive in the less aggressive carcinoid and atypical carcinoid tumors, whereas greater than 50% staining is expected in large cell neuroendocrine carcinomas and small cell carcinomas. A more definitive diagnosis may be made after evaluating histologic features of the resected tumor.
The prognosis for typical carcinoid tumor is excellent because metastasis is rare and slow to occur. Surgical resection of the tumor leads to 5-year survival rates of over 90 percent. The patient in this case has elected for surgical resection of his tumor and is scheduled for surgery.
References:
Chesnutt AN, Chesnutt MS, Prendergast NT, Prendergast TJ. Pulmonary Disorders. In: Papadakis MA, McPhee SJ, Rabow MW. eds. Current Medical Diagnosis & Treatment 2019 New York, NY: McGraw-Hill; http://accessmedicine.mhmedical.com.libproxy1.usc.edu/content.aspx?bookid=2449§ionid=194434470. Accessed September 19, 2019.
Cibas ES, Ducatman BS. Cytology: Diagnostic Principles and Clinical Correlates. Fourth Edition. Philadelphia, PA. Elselvier Saunders. 2014.
Hendifar, Andrew E., Alberto M. Marchevsky, and Richard Tuli. “Neuroendocrine tumors of the lung: current challenges and advances in the diagnosis and management of well-differentiated disease.” Journal of Thoracic Oncology 12.3 (2017): 425-436.
Okike, Nsidinanya, Philip E. Bernatz, and Lewis B. Woolner. “Carcinoid tumors of the lung.” The Annals of thoracic surgery 22.3 (1976): 270-277.
